3100 Tongass Ave.
Ketchikan, AK 99901
Nonpro t Org.
U.S. Postage
PAID
Ketchikan, AK
Permit No. 13
H E A L T H C A R E A N D W E L L N E S S I N F O R M A T I O N F O R O U R C O M M U N I T Y
S P R I N G 2 0 1 4
FIND US ON FACEBOOK
Like us on Facebook for an easy way to stay up-to-date with
the latest news and events at PeaceHealth Ketchikan Medical
Center. Just visit
.
Facebook “f”Logo
CMYK / .ai
M
ost people wouldn’t consider losing
. million in revenue an e ective way
to run a business. Matt Eisenhower
isn’t one of those people. For him and other
caregivers at PeaceHealth Ketchikan Medical Center, this
is a new way to de ne success. Matt is ProgramManager
for the Centers for Medicare & Medicaid Services (CMS)
Innovation Grant awarded to PeaceHealth Ketchikan in
. His work is part of a dramatic philosophical change
in health care delivery that has successfully saved local
patients about . million in the last year and a half.
Payments to PeaceHealth are down percent, hospital
readmissions between two and four months after
discharge are down percent, and there is improvement
in patients with chronic conditions like diabetes and high
blood pressure.
A BROADER VISION
While at rst glance it may look
as if Matt’s job is to decrease revenue for PeaceHealth
Ketchikan, the real purpose is to nd innovative ways to
provide better care, which leads to better health, resulting
in lower costs.
“Hospital-based health care costs continue to go up, and
the way insurance companies and government pays for
this care is changing dramatically,” Matt says. “For decades,
American health care payment models have been heavily
weighted toward xing problems in the hospital setting.
is has been the emphasis of health care, and it’s what
primarily drives health care payments now. We are on the
cutting edge of developing di erent models that reward
hospitals and clinics for e ective preventive care.”
e centerpiece of the grant is care coordination, which
provides ongoing care and contact with patients who
have been discharged from the hospital or who live with
a chronic disease. New sta has been hired to implement
the program. rough the three-year, . million grant,
PeaceHealth Ketchikan has hired three registered nurses,
a licensed practical nurse, a social worker, a clinical
educator, a nurse practitioner, and a manager. Ten other
positions are partially funded through the grant.
Here’s how it works: When patients leave the hospital
and return home, a nurse or the social worker calls to talk
about the patient’s progress and answer any questions.
is care coordinator asks questions too and, most
important, listens. Earlier this year, a patient remarked
in conversation that there was some warmth near the
surgical site and that the patient planned to tell the
surgeon during a follow-up appointment the next week.
Instead, because of care coordination, that patient was
seen almost immediately, and what could have become
a major infection was an easily treatable condition.
In the last quarter of
, about percent of the more
A different
measure of success
KEEPING
CARE IN THE
QUOTIENT
“It’s not about revenue alone, but about healthier
people and fewer people in the hospital.”
than
patients discharged were contacted. Intervention
at that time resulted in an approximate decrease of
percent of immediate readmissions. “What that means,”
says Matt, “is that three or four patients every month were
not returning to the hospital.”
PROOF POSITIVE
For people with chronic conditions like
diabetes or congestive heart failure, a care coordinator
helps monitor their condition, makes appointments, and
otherwise helps overcome hurdles to care.
It’s no secret that some people avoid colonoscopies
and mammograms. With the encouragement of care
coordinators, more people are being reassured that the
tests aren’t horrible (they really aren’t) and are being
screened for breast cancer and colorectal cancer.
Particularly encouraging is a big uptick in
immunizations. From a baseline of percent in November
,
percent of people now have the appropriate
immunizations.
But what about all that lost revenue?Matt has the answer.
“ is is what we celebrate,” he says. “It’s not about revenue
alone, but about healthier people and fewer people in the
hospital. is is deep in the DNA of PeaceHealth and the
people who work here. is is good medicine, it’s the right
thing to do, and ultimately the path toward balancing
revenue and costs by reducing unnecessary return trips to
the hospital for expensive care.”
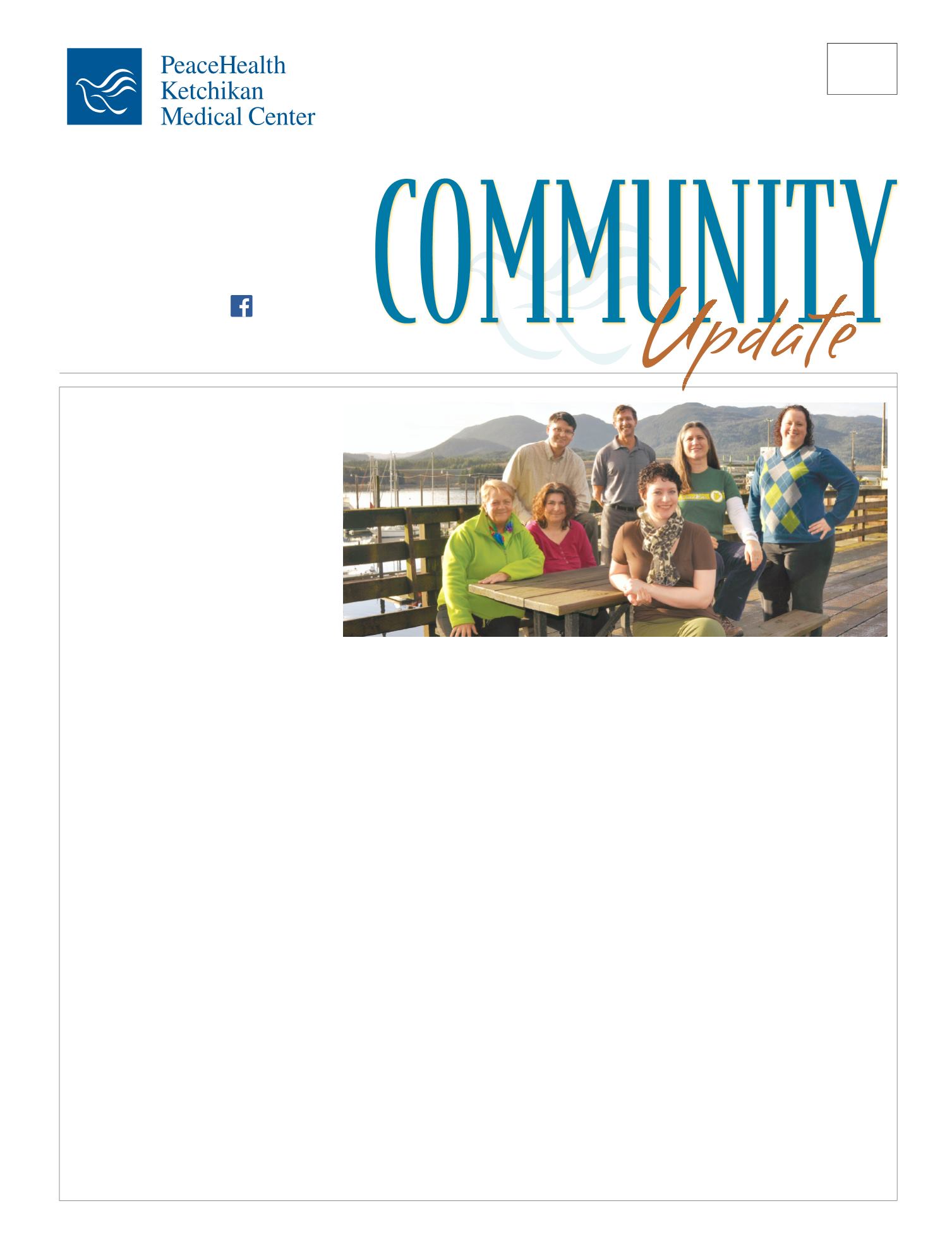
A CARING TEAM: From left, Jamie Easterly, RN, Care Coordinator; Michele Cornwall, RN, Clinical Educator; Matt
Eisenhower, Program Director; Ken Tonjes, Chief Administrative Officer; Caitlin Andrews, Clinical Social Worker;
Lisa McCranie, LPN, Care Coordinator; and Amanda Glanzer, RN, Pediatric Care Coordinator. Not pictured: Andrew
West, RN, Care Coordinator, Craig Clinic; and Michele Budd, Regional Vice President for Ambulatory Services.
—Matt Eisenhower, PeaceHealth Ketchikan
The project described was supported by Grant Number 1C1CMS330966 the
U.S. Department of Health and Human Services, Centers for Medicare & Medicaid
Services.
The contents of this publication are solely the responsibility of the authors and do not
necessarily represent the of cial views of the U.S. Department of Health and Human
Services or any of its agencies.